-
Do Compassion Rounds Improve Professional Quality of Life for Nurses ?
Deepti Bhatnagar and Martha E.F. Highfield
Background: When RN worklife quality is positive, nurse and patient outcomes are positive (e.g, RN retention and patient satisfaction), and when worklife quality is negative, outcomes are negative (e.g., RN disengagement and errors).Yet professional quality of life(QOL)among RNs in progressive care units (PCUs) is undocumented. Stamm’s framework of compassion satisfaction and fatigue guided this study. Purpose: The purpose was to test the effect of supportive groups on professional quality of life. The hypothesis: Compassion Rounds (CR) will improve compassion satisfaction and reduce compassion fatigue among PCU RNs. Methods/ design: Using a quasi-experimental design we measured RNs’ professional QOL once before and once after CR using the well-established ProQOL—a30-item, self-report instrument that yields 3 ordinal subscale scores: Compassion Satisfaction (CS), Burnout (BO), and Secondary Traumatic Stress (STS).Paper-and-pencil demographic sheets and ProQOLs were coded for paired analysis. Return of confidential questionnaires documented consent. After initial data collection, Palliative and Spiritual Care staff facilitateda10-week CR intervention consisting ofbiweekly,30-45 minute, simultaneous live/online, open-ended discussions with staff RNs. Meetings focused on challenges enacting the RN helper role. The sample was an inclusive one of85PCU RNs in a 377-bed, Magnet-recognized, nonprofit facility. Results: Overall response rate was high (44%; N=39). Eighteen (18) respondents attended CR between 1 and 10 times (M= 3). Mean age was 35, and a majority reported female gender(89%), BSN preparation (75%), and no specialty certification (74%). Respondents were ethnically diverse. Using ProQOL cut scores, 7 individuals reported high STS; the remainder reported moderate to low BO, STS, and CS. Inferential t-testing of paired pre/post ProQOL scores (n = 10pairs) showed a pre-CR to post-CR rise in both BO (pre M = 23; post M = 28) t(8) = -2.3, p = .05 and STS scores(pre M = 22; post M = 33) t(8) = -3.5, p = .008. CS subscale scores decreased(pre M = 28; post M = 18) t(8) = 3.7, p = .005. Independent t-testing using all data yielded similar results (p < .05). The hypothesis was rejected. Conclusions: RN professional QOL deteriorated during CR, but no counterfactual exists; CR may have prevented worse outcomes. The PCU housed COVID-19 patients, and data were collected during peak hospitalizations. Moreover, completing ProQOL could have increased respondent self-awareness, and 10 weeks of CR may have been long enough to raise issues without resolving them. ProQOL scores are screening only and so must be cautiously interpreted (Stamm, 2010). Implications: Implications include a need for staff-identified strategies for group empowerment, as well as attending to individual risks for depression, PTSD, or burnout. RNs can access the free ProQOL to aid in guided career counseling. Moreover, further CR and PCU RN studies are warranted. For example, post-pandemic ProQOL data from the same PCU population might differentiate persistent downward trends from transient, self-resolving ones
-

Feasibility of launching a multi-state nursing health study in the midst of the COVID-19 pandemic
Ross Bindler, Shaekira Niehuser, Trisha Saul, and Teresa Bigand
Background: The Quadruple Aim recommends that healthcare institutions support clinician well-being as a strategy to improve patient and caregiver outcomes. During the COVID-19 global pandemic, Registered Nurses (RNs) working full-time, 12-hour shifts have reported increasing health concerns. Therefore, research documenting objective information on preventive health habits of RN’s is needed to support nursing well-being. Yet, conducting bio-behavioral research in this population, especially during the pandemic, presents with unique challenges. Purpose: The purpose of this pilot study to assess the feasibility of collecting and evaluating health data from RNs working full-time, 12-hour shifts across the United States during the COVID-19 pandemic. Methods/Approach: This observational descriptive study recruited 12-hour shift RNs working in a large health system in the United States. RNs wore a wrist actigraph for 10 days, maintained a seven-day electronic food diary, tracked daily step counts using a wrist pedometer, and optionally provided two stool samples for sequencing analysis. Nurses completed an online screening form to assess for study eligibility, and were contacted by a research team member to provide consent if they met eligibility criteria. Research staff created and shared a digital workbook to explain the protocol as well as an interactive online course to provide standardized education on completing electronic food diaries. Participants were mailed devices for tracking health habits. Research staff were available to participants via phone call or email to answer questions at any point during the study. Participants were invited to complete an optional post-study feedback survey to describe the experience of being involved in the study. Recruitment began in October 2020 and the study is still open for participant enrollment. Results: At this time, 82 nurses met study criteria and 49 consented to participate (n=27day shift and n=22night shift). Of these, 37 volunteered to provide a stool specimen. Of the consented nurses, a total of 5 have withdrawn for reasons such as family or school issues. Out of 32 nurses who have completed the study, 22 provided a stool specimen, 2 forgot to collect despite consenting, and9 nurses provided feedback where 66% reported reviewing the online module course. Of those who completed the study, 100% successfully captured sleep data using the wrist actigraph, yet 15.6% required research staff assistance with documenting some aspect of the food diaries. Conclusion: Preliminary findings suggest that it is feasible for nurses to provide objective health information in the context of working full-time, 12-hour shifts during a global pandemic. Future work is needed to understand best strategies for conducting bio-behavioral research among RNs providing direct patient care in the hospital setting. Implication to Practice: Research is needed to characterize health habits of nurses, particularly those providing full-time, direct patient care, to support caregiver well-being and facilitate optimal patient outcomes. Preliminary findings suggest that while barriers exist that restrict nursing involvement in bio-behavioral studies, especially during the pandemic, nurses may successfully participate in studies which could leverage understanding of short and long-term health needs for this population.
-

Utilizing a Social Media Platform to Increase Participation in a Virtual Journal Club
Alex Bubica and Trisha Saul
Background: A virtual journal club (VJC) is a place where nurses can read, synthesize, and discuss research and evidence-based practice articles. There is a well-known time lag of disseminating this knowledge from bench to bedside. In 2016, a 300-bed community hospital constructed a VJC to educate nurses on the latest studies. In 2016 and 2017, this VJC was used via an intranet-based platform with little success. Main barriers included (1) no access outside of work and (2) difficulty following threads leading to in-cohesive interactions. In 2018, a website was created. This platform had one fatal flaw, a multistep verification process to gain access, with the verification email being routed into spam. In late 2018, a literature search was done to identify best practices. A number of articles were reviewed with results indicating that the utilization of a social media platform increased participation.
Purpose/Aim: The purpose of this evidence-based practice project was to offer a social media platform for all nursing staff to participate in a VJC. Aim 1: To set up an organizationally approved social media account for the VJC. Aim 2: For the participants to have access to the VJC at home and at work. Aim 3: To increase the number of participants using the VJC.
Approach: The Nursing Research Council used the Rosswurm and Larrabee model as a systematic evidence-based practice process. Step one, assess the need for change, was done mid-2018 when platform problems were identified. Steps two and three: link problem with interventions and outcomes, and synthesize best evidence, was done at the end of 2018. Step 4, design a plan, was discussed in detailed early in 2019, and a number of traditional social media platforms were reviewed but did not meet institutional security measures. One social media platform that the organization already used was identified. Step 5, implementing and evaluating a plan, involved three phases. Phase one was exploratory. An account was created with basic information. Council members and the Education team were invited to test out the accessibility (i.e., desktop and phone application). Phase two included a soft-opening with the VJC completely set up, and Council members each did an initial post and a response. All potential barriers were evaluated and addressed. Phase 3, hospital go-live in May, included a number of promotional techniques (i.e., QR codes, emails, signs). Stage 6, integrate and maintain is discussed below.
Results: Aim 1 and Aim 2 were successfully met by identifying a user-friendly social media platform, that resembles the basic principles of a traditional social media news feed. Aim 3 was measured by number of total members and posts. Compared to 2018, 2019 increased in VJC members from 22 to 44 and total number of posts from 46 to 106.
Conclusion & Implications: Advances in nursing practice need to be communicated quickly. Utilizing a social media platform versus an internet-based platform has increased participation within the VJC. Thus this practice change has been deemed successful, and continues to be maintained by the Nursing Research Council.
-

The Impact of the Implementation of Code-Blue Nurse Champions for Cardiac Arrest
Beverly Holland and Sherri Mendelson
Background: Delayed recognition of in-hospital cardiac arrest (IHCA) events can affect survival rates. At the project site, there was a failure to rescue in the medical-surgical population. Key elements of success include staff identifying at-risk patients combined with early interventions to prevent deterioration of cardiac arrest. Survival and favorable outcomes for IHCA (i.e., neurological sequelae) were shown to be highly dependent on several factors, such as a skilled resuscitation team, prompt initiation of cardiopulmonary resuscitation and defibrillation, and organizational structures to support resuscitation care; therefore, nurses are an integral part of an IHCA response.
Purpose / Aims: The purpose of this quantitative quasi-experimental quality improvement project was to determine if the implementation of Banks and Trull's code blue nurse champion role (CBNCR) would impact the nurses' knowledge and self-efficacy regarding cardiopulmonary resuscitation and patient IHCA survival rates at an acute care hospital in Southern California over four weeks. Bandura's self efficacy theory and the trans-theoretical model were theoretical underpinnings of the project.
Methods / Approach: A quantitative methodology was selected for this project to discover through statistical analysis, quantifiable, objective data related to the implementation of CBNCR on nurses' self efficacy to respond to cardiac arrest and survival of patients suffering IHCA before and after the intervention. The training for the CBNCR included IHI rapid response education and in-situ simulation on cardiac arrest scenarios. Results: Data on nurses' (N=18) cardiac arrest knowledge and self-efficacy were evaluated using the Knowledge and Attitude of Nurses in the Event of a Cardiopulmonary Arrest instrument. A paired t-test showed no statistically significant improvement in nurses' knowledge (p=.959) and self-efficacy (p=.910). The total patient population was 302, n=147 in the comparative (n=2 IHCA) and n=155 (n=1 IHCA). To analyze IHCA, a Fischer's exact test was used, which was not statistically significant (p=.667) (pre n=2, 50%; post n=1, 100%).
Discussion: Results indicated the CBNCRs may not improve nurses' knowledge and self-efficacy or IHCA rates. Although not statistically significant, clinical significance was demonstrated as the CBNCRs provided skills to improve early recognition of impending IHCA and enhanced nursing staff's awareness of patient's deterioration.
Conclusion: Simulation offers acute care nurses an opportunity to practice life-saving techniques in the clinical setting without patient harm. Simulation as a safety strategy focuses on developing positive attributes and productive capacities that underpin safety performance. Implementing dedicated nurse champions is a novel approach to improve recognition and response to deteriorating patients. Providing additional hands-on experience through cardiac arrest in-situ simulation could equip them to provide timely and effective CPR during cardiac arrest.
Implications for practice: The results provide insight into the innovative role of code blue nurse champions. Implementation of the CBNCR is predicated on providing educational training to a core group of medical-surgical nurses on rapid response roles, how to activate RRT, development of SBAR communication, and in-situ simulation on cardiac arrest. The recommendation for practice is to replicate and implement nurse CBNCRs throughout the medical-surgical units. Creating a hospital-wide CBNCR position may decrease nurses' anxiety, while increasing self-confidence and self-efficacy in recognizing patient deterioration and early initiation of CPR.
-

How Much is too Much: Examining Fluid Responsiveness in Septic Patients
Natalie Kitago, Lak Tuong, and Sarah Rosenberg
Background & Significance: The leading cause of death of critically ill patients is sepsis. The CDC reports that sepsis is estimated to be responsible for 1 of every 3-hospital deaths. Furthermore, in hospitals located in California for one large hospital system, a reported30.74% patients admitted to the ICU with sepsis died in the year 2017.
Purpose: The purpose of the study was to determine if utilizing non-invasive pulse contour technology (PCT) is a feasible intervention to manage fluid responsiveness and resuscitation specifically with septic patients in a community Intensive Care Unit in California. A secondary aim was to determine if use of PCT and a nurse-driven algorithm for fluid resuscitation could improve patient outcomes with respect to mortality rate, ICU length of stay in days, and ICU ventilator use days.
Methods: A single-cohort feasibility study with 50 participants was conducted. Subjects were admitted to ICU directly from the Emergency Department with primary diagnosis of sepsis/septic shock, and enrolled within 24 hours of admission. Subjects had the Pulse Contour Technology applied, remaining in place for 72 hours or until discharge from ICU. A nurse driven algorithm was utilized to determine when the patient was to be given IV fluids verses starting vasopressors based on fluid responsiveness. Retrospective and prospective data was collected using specific inclusion and exclusion criteria. A certified statistician consulting with our hospital analyzed all data using standard SPSS software.
Results: Out of the 50 patients enrolled in the prospective study the algorithm was applied 92.3% of the time. This indicates that a nursing driven protocol for fluid management is feasible in the community hospital ICU setting. We found that the PCT did guide fluid resuscitation. When comparing the prospective data to the retrospective data we found that mortality decreased from 31% to 22%, ventilation days decreased from 5.3 to 1.3, and length of stay decreased from 6.4 to 3.2 days. Finally, we assessed the prospective data, finding that 62% of patients were considered fluid overloaded per definition. There was no statistical significance between fluid overload and procedures performed.
Conclusion: Utilizing PCT and algorithm to guide fluid management in sepsis patients to determine if a patient needs vasopressors verses fluids demonstrated positive outcomes. Going further it can assist in bed selection from ER, or RRT; identifying if septic patient requires ICU for vasopressor therapy or step down unit for further fluid resuscitation. It would be beneficial to conduct a larger scale study to determine if the results translate beyond our community hospital setting.
-
The effect of COVID-related changes in diet, exercise, sleep patterns, and mood on stress levels of RNs who work 12-hour shifts during the pandemic
Amber Norman, Trisha Saul, Ross Bindler, and Teresa Bigand
Background: Registered Nurses (RNs) working 12-hour shifts are regularly exposed to high stress situations which has intensified during the COVID-19 pandemic. Chronic stress exposure may lead to changes in health habits and impact sleep, exercise or diet, augmenting risk for adverse health outcomes and taking a negative emotional toll. While nursing staff educate patients on reducing stress and engaging in health promotion behaviors, there is little research on perceived stress and relationships to COVID-related changes in sleep, diet, exercise, and mood of nurses working full-time, 12-hour shifts during the pandemic.
Purpose: The purpose of this pilot study was to gain preliminary insight on perceived impacts of the COVID-19 pandemic on exercise, sleep, diet, mood, and stress in 12-hour shift RNs.
Methods/Approach: This observational descriptive study was composed of 12-hour shift RNs in the Western United States. This is an ongoing pilot study with the end goal of 60 participants. RNs completed surveys providing self-reported information on demographics, stress, and emotional and behavioral changes perceived in relation to the COVID-19 pandemic. Stress was measured with the valid and reliable Perceived Stress Scale short form, and author-created Likert scale questions evaluated whether diet quality, sleep quantity, sleep quality, exercise, stress, sadness, or anxiety worsened, remained unchanged, or improved since the onset of the COVID-19 pandemic. Data were analyzed using descriptive and frequency statistics as well as independent samples t-tests in SPSS version 26.
Results: At the time of preliminary analysis, 40 participants provided data on the variables of interest. Of these participants, there were no observed significant differences among self-reported stress levels when comparing: shift worked (night versus day); COVID-related exercise, sleep, anxiety, or stress changes; age; or gender. One significant preliminary finding was that RNs who reported worsening dietary habits related to COVID tended to have increased stress levels (p=0.005). Another finding was that higher levels of stress were reported among nurses with greater-perceived personal sadness related to the COVID pandemic (p=0.003).
Conclusion: RNs are called to help others yet may be at risk for high stress and poor health outcomes, especially in the context of working during the COVID pandemic. These preliminary data suggest trends in relationships between stress and self-reported COVID-related changes to dietary habits as well as personal sadness among RNs.
Implication to Practice: Nurses are front-line caregivers and optimal physical and emotional health is critical to delivering effective patient care. While this small pilot study is ongoing and acknowledges that these are preliminary findings, it is suggested that working full time, 12-hour shifts in the hospital setting during the pandemic may have an impact on stress of RNs which could negatively influence well-being.Future studies may benefit from more directly exploring relationships between diet, mood, and stress levels over time in this population.
-

Improving Outcomes for Pregnant Women with Severe Hypertension
Danette Schloeder
Background: In 2019, a large hospital in Alaska joined the Alaska Perinatal Quality Collaborative (PQC). The first project was the AIM Hypertension Project. The goals of the project were to reduce severe maternal morbidity among preeclampsia cases by 20% and Increase the timely treatment of hypertension to 80%. Other process and structure measures included education, simulation, clinical debriefs, and follow-up visits.
Methods/Approach: The PQC used monthly educational sessions, data collection and review of every case with severe hypertension, and Plan-Do-Study-Act cycles. Data collection occurred over an 18-month period. Cases were identified by the Washington State Hospital Association database and reviewed for timely treatment of severe hypertension. Timely treatment is defined as either a systolic BP of equal to or greater than 160mmHg or diastolic equal or greater than 120mmHg that persists for greater than 15 minutes. The patient must be treated with an anti-hypertensive within 60 minutes of the first blood pressure.
Results: Data collection occurred from July 2019-December 2020. A total of 225 cases were reviewed. The 2020 rate of timely treatment of severe hypertension increased to 81.3% (Goal of 80%). The project was able to reduce the variation in practice. There were three months with 100% timely treatment. In measuring the Severe Maternal Morbidity from Pre-eclampsia cases, the 2019 rate was 8.4%. The2020 rate was 6.9% (Goal 6.72%). The PSJH overall rate was 8.7%.
Conclusions: This project was able to standardize the processes around the management of severe hypertension through order sets, standards of work, education, simulation, and EPIC alerts. This large hospital implemented bedside debriefs and quarterly case reviews of cases that resulted in severe maternal morbidity.
Implications for Practice: This project demonstrated the power of working collaboratively with the statewide PQC to improve patient outcomes. There were significant challenges with COVID-19 priorities and distractions. Overall, both nurses and physicians are committed to timely treatment and the reduction of severe maternal morbidity.
-

HAPI- Related BIPAP in DSU
Carmyle Seville and Angelica Taneca
Background: Most medical-device related pressure injuries develop when skin or underlying tissues are subjected to a sustained pressure or shear from medical devices. Dressings have shown substantial biomechanical effectiveness in alleviating facial tissue deformations and stresses by providing localized cushioning to the tissue at risk. Our units (DSU and SDU) provide for the monitoring and care of patients with moderate or potentially severe physiologic instability requiring technical support but not necessarily artificial support such as patients on BIPAP management. In the 4 months (June-Sept 2019) before the project initiation, one patient per month had BIPAP related pressure injury.
Purpose: This Hospital Acquired Pressure Injury Improvement was initiated to reduce and eliminate BIPAP related pressure injuries using evidence-based solutions and to identify problem areas promptly for early treatment and prevention.
Methods/Approach: Design: Evidence-based Practice Setting: DSU and SDU Participants for clinical outcomes: Patients using BIPAP Procedures: Historic data was obtained from leadership. Unit nurses acquired curagel nasal silicone pads and engaged respiratory therapy in the project. Staff members were educated in new procedures: alternating mask use between full mask and total face mask every 6 hours, incorporating skin assessment under medical device during 4 eyes, Skin Braden Scores, use of silicone pads, documentation of HAPI. Random chart audits were done to evaluated compliance and clinical outcomes. Results: Between October 2019 through March 2020, there were no BIPAP related HAPI and audits demonstrated 100% compliance on all measures.
Conclusion: Alternating face masks, and application of silicone pads were effective in eliminating pressure injuries related to BIPAP use. Under normal conditions, the interventions produced complete elimination of pressure ulcer.
Implications for practice: Application of evidence to a significant care issue resulted in zero occurrence of BIPAP-related HAPI from October 2019 to March 2020. Audits will continue to help keep project on track. Education and re-education will be done as needed for continued success.
-

Improving Discharge Times and Patient Flow
Robyn Song, Miguel Ros, August Maggio, Kim Nicole Rossillo, Jason Caberto, Soudi Bogert, Stephanie Floriano, Caroline Brandenburger, Darleen Nguyen, Jacoba Walsh, Richard Urgel, Tanya Lenhardt, and Joan Aquino
Background: Delays in discharging patients can impact hospital and emergency department (ED) throughput. The complex discharge process makes it difficult to ensure that patients are set up for successful post-hospital care regimens. The focus of this project was to improve discharge times and flow throughout the hospital to align with national standards of providing the right care, in the right place, at the right time. To improve access to beds, The Joint Commission stipulates that hospitals have processes in place to support patient flow throughout the hospital and to use data to drive improvements in patient flow. Failure to regulate flow puts patients at risk for harm and less than optimal care. It also increases clinician burden which may accelerate burnout. A lack of optimal patient flow results in ED boarding and diversions, long waits, and boarding in post-anesthesia care units.
Purpose: The purpose of this project was to improve overall patient throughput within one large acute care hospital by improving discharge times. Baseline discharge times averaged over 4 hours with less than 15% of patients being discharged in less than 2 hours.
Methods: A multidisciplinary patient flow team was charged with improving discharge times and removing barriers to timely discharges. The team consisted of representation from executive leadership, nursing management, pharmacy, physician staff, case management, and frontline staff. Meeting weekly, the team rapidly instituted small tests of change to address the barriers to timely discharges. The Admission Discharge Team facilitated education. Discharge accountability teams on nightshift assisted with preparing patients for discharge. Case Manager/charge nurse rounds were instituted to identify patients ready for discharge and anticipated barriers. Electronic whiteboards were utilized for interdisciplinary communication. Discharge times were reported weekly in a public area on units.
Results: The program resulted in an increase in caregiver engagement in discharges and discharge times. Readmission rates decreased for heart failure patients to below national benchmark. Discharges completed in less than 2 hours improved to almost 30%. Average discharge times decreased from 4 hours to 2 hours and 30 minutes. Also, responses improved to the patient satisfaction question "When I left the hospital, I had a good understanding of the things I was responsible for in managing my heath:" by 25%. Conclusions: Discharge planning that is initiated on the day of admission and addressed ongoing in a uniform fashion by both nursing shifts and ancillary caregivers can alleviate delays on discharge day. An improvement in discharge times improved hospital flow. A focused approach on education throughout the patients stay improved their ability to manage their health at home and reduced readmits.
Implication for Practice: The discharge protocol and procedures will continue to be implemented and evaluated for improvement needs and barriers and expanded to include skilled nursing facility transfers. The discharge process has been implemented in several inpatient units. Discharge times/barriers will be re-evaluated quarterly and the focused patient flow team will make additional adjustments to make the discharge process more efficient.
-
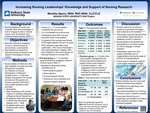
Increasing Nursing Leaderships’ Knowledge and Support of Nursing Research
Marietta Sperry
Background: The lack of leadership support and research knowledge are reported barriers nurses experience in conducting hospital-based research.
Purpose/aims: The purpose was to determine if nursing leadership's knowledge and support of nursing research could be improved through an interactive intervention and to identify their research needs.
Methods/Approach: Design: A translational research study (Doctor of Nursing Practice project) utilizing the Barriers to Nurses' Participation in Research Questionnaire was conducted. Sample: The sample consisted of an even distribution of managers/assistant managers, charge nurses, and directors/chief nursing operating officers. Of the 300 email invitations, 17 nursing leaders completed the pre-test and eight completed the post-test. Setting: Six hospitals within a large health care system in the United States consented to have their nursing leaders receive an email invitation to participate. Intervention: Nursing leaders were provided links for a pre-test, an interactive learning module on clinical scholarship (nursing research), and a post-test. Time frame: Surveys were collected August 19-October 14, 2020. Data: Demographics typical of nurses was collected, such as age, education, position, years of employment, along with perspectives of barriers to nursing research. The Barriers to Nurses' Participation in Research Questionnaire (BNPRQ) provided the basis for the data. The BNPRQ asked which barriers the nursing leader experienced such as lack of time, knowledge, mentors, infrastructure, incentives, nursing research council, leadership support, and training. Participants were given the opportunity to provide some qualitative answers. Paired and un-paired t-tests, descriptive statistics, and a qualitative analysis were performed.
Results: The pre-test group (n = 17) breakdown of nursing leaders was 5 CNOs/directors, 7 assistant managers/managers, and 5 charge nurses. The post-test group (n = 8) consisted of 3 CNOs/directors, 3 assistant nurse managers/managers, and 2 charge nurses. The Pre-test group (n = 17) cited "lack of time" as the number one barrier. Nearly 50% felt a lack of knowledge hindered, and 52.96% either strongly agreed or agreed that the intervention improved their research knowledge. Near this same percentage agreed that lack of time, mentors, and resources also hindered their ability to support or conduct research. However, in the qualitative portion, a lack of leadership support, lack of data collection/tools, need for a hospital-based nurse research mentor, and guidance for developing research inquiry were identified as gaps.
Conclusion: Nursing leaders in this sample reported many of the same barriers that front-line nurses experience including a lack of leadership support for engaging in research. The educational intervention improved nursing leaderships' knowledge and support of nursing research in half of the respondents.
Implications for practice: Hospitals may benefit from providing nurse leaders the basic tools of research, local leadership support, technical advising, and a designated nurse researcher contact in order to facilitate and support nursing research.
-

Blind Taste Testing: A Case Study of an Emergency Room RN with Covid-19 Anosmia & Hypogeusia (Loss of Taste & Smell)
Marietta Sperry and Kimberly Kohlieber
Background: Anosmia, or the loss of taste and smell, is an important symptom for nurses to screen for among patients, as this can result in a poor appetite which impairs healing. In the early stages of the COVID19 pandemic, anosmia was not a known symptom indicative of infection with the virus. Yet, one Registered Nurse who was working in an Emergency Room received a positive COVID test following a workplace exposure to the virus while wearing personal protective equipment, and began to complain of anosmia shortly thereafter. Because the anosmia persisted, his spouse conducted blind taste test on him in their home with various spices, flavors, and fruits. The nurse subsequently posted about the experience on social media.
Purpose: The purpose of this case study is to describe one healthcare provider's experience with anosmia associated with a confirmed positive Sars-Cov-2 diagnosis.
Methods: An individual case study was conducted on a Healthcare provider with a confirmed positive COVID diagnosis early in the year 2020 during the COVID pandemic. The individual was a male who was employed as an emergency room Registered Nurse. He was not on any medications or supplements, reported no past medical conditions, and received no treatment or hospitalization during the period of anosmia. The nurse’s spouse blindfolded him and administered an array of spices, flavored liquids, and fruits, asking him to distinguish what he was tasting and smelling. The spouse then recorded all responses and posted results to social media. The project lead of this case study reviewed the information on the social media post, contacted the couple, and received permission to more widely share the findings.
Results: Based on information posted on social media, the nurse was unable to distinguish various spices, or liquid flavorings. While the nurse was able to identify fruits based on texture, he could not detect any distinct flavors such as sweetness. The nurse reported, “I cannot smell a thing; everything tastes bland. Conclusion: Blinded taste-testing is a feasible and low-cost method for confirming the symptom of anosmia among those who may be infected with the COVID virus. Future work should focus on supporting affected individuals with anosmia to maintain healthy nutritional intake despite the absence of taste and smell while ill.
Implications for Practice: Taste and smell deficiencies may occur with SarsCov-2 infection. Nurses should be screen for this symptom among patients and recommend COVID-testing where appropriate to drive early intervention and treatment of the virus. Additionally, because taste and smell normally help drive appetite, nurses should assess for deficiencies in nutritional intake among individuals with anosmia to support a healthy diet for optimal healing.
Printing is not supported at the primary Gallery Thumbnail page. Please first navigate to a specific Image before printing.




